Vitamin D
CAS number: 1406-16-2
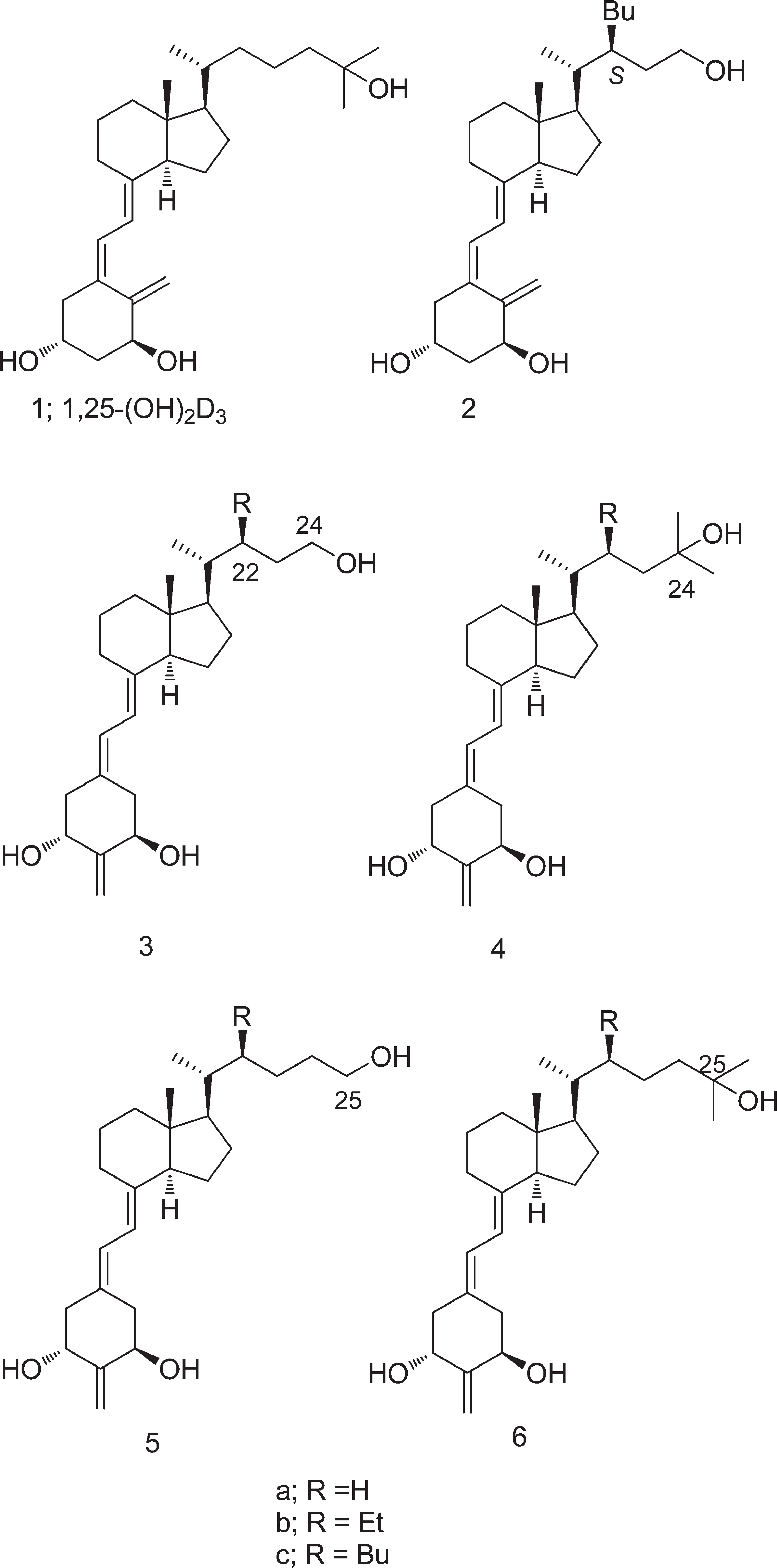
Vitamin D ultimately comprises a group of lipid-soluble secosteroids responsible for a variety of biological effects, some of which include increasing the intestinal absorption of calcium, magnesium, and phosphate. With reference to human use, there are 2 main forms of vitamin D - vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol).
Related images
Related Questions and Answers
A: Vitamin D binds to VDRs, forming a heterodimer with RXR, which translocates to the nucleus and regulates genes related to muscle cell proliferation, differentiation, and metabolism. Non-genomic pathways involve modulation of MAPK, PI3K/Akt, and PKC signaling, enhancing muscle excitability, insulin sensitivity, and antioxidant defenses.
A: Low serum 25-hydroxyvitamin D (25(OH)D) levels are associated with reduced muscle strength, physical performance, and increased sarcopenia prevalence. Mechanistically, vitamin D deficiency impairs muscle protein synthesis, disrupts calcium homeostasis, and increases oxidative stress and inflammation, exacerbating muscle deterioration.
A: Beyond its classical role in bone metabolism, vitamin D acts as a prohormone with pleiotropic effects, including modulation of gene expression in skeletal muscle via vitamin D receptors (VDRs). It regulates muscle protein synthesis, calcium homeostasis, mitochondrial function, and inflammatory signaling through genomic and non-genomic pathways.
A: Poel et al. (2012) and Eggemoen et al. (2018) found that even after adjusting for BMI, vitamin D deficiency remained independently associated with GDM, suggesting obesity exacerbates but does not fully explain the risk.
A: Parlea et al. (2012) and Lau et al. (2011) found that winter months were associated with lower 25(OH)D levels and higher GDM risk, while summer showed the opposite trend.
A: Studies (Nobles et al., 2015; Lau et al., 2011) found that ethnic minorities (e.g., Hispanic, Middle Eastern, African descent) had lower 25(OH)D levels and higher GDM risk, likely due to reduced cutaneous vitamin D synthesis.
A: Results are mixed. Yap et al. (2014) found that high-dose vitamin D supplementation (5000 IU/day) did not improve maternal glucose levels, but prevented neonatal vitamin D deficiency. Shahgheibi et al. (2016) reported reduced GDM risk in high-risk women supplemented with vitamin D.
A: A dose-response meta-analysis by Sadeghian et al. (2020) found that each 10 nmol/L increase in 25(OH)D was associated with a 2% reduction in GDM risk (effect size: 0.98; 95% CI: 0.98–0.99). Women with levels <50 nmol/L had a significantly higher GDM risk.
A: Vitamin D influences glucose metabolism by interacting with pancreatic β-cell vitamin D receptors (VDRs), enhancing insulin secretion and improving insulin sensitivity through calcium-dependent signaling pathways. Deficiency leads to insulin resistance and increased GDM risk.