Phenobarbital
CAS number: 50-06-6
Phenobarbital is a member of the barbiturate drug class that holds versatile therapeutic applications. This drug is effective in anti-seizure management, treatment for status epilepticus, and insomnia; it also plays a pivotal role in addressing benzodiazepine and alcohol withdrawal. Phenobarbital (phenobarbitone) was first used as an antiepileptic drug 100 years ago, in 1912.
Related images
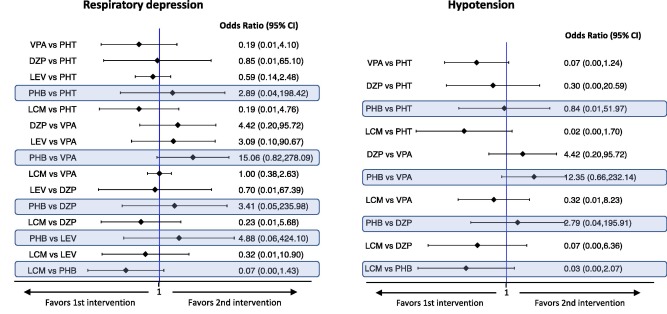
Interval plots for the safety outcomes of five studies in benzodiazepine-resistant Status epilepticus. Highlighted in blue are the comparisons including phenobarbital (From: Brigo et al. Epilepsy and Behavior 2019).
Related Questions and Answers
Q: How does phenobarbital penetrate the brain during status epilepticus compared to a healthy brain?
A: Preclinical studies and human trials suggest that brain uptake of phenobarbital in status epilepticus is much faster than in the healthy brain. This faster entry into the brain during status and preferential concentration for a long time is attributed to hyperperfusion in the early stages, systemic hypertension with increased mean arterial pressure, and a decrease in pH due to metabolic acidosis and lactate accumulation. Maximum brain concentrations were reached at 3 minutes with phenobarbital, compared to 1 minute with diazepam and 6 minutes with phenytoin in cat brain studies.
A: Mechanism of action: Potentiation of GABA(A) receptor-mediated inhibition by prolonging periods of Cl channel opening; inhibition of AMPA-ergic glutamate receptors; at high doses, inhibition of rapid-firing voltage-gated Na-channels.
Bioavailability: Intravenous: 100%; Intramuscular: 101 ± 11%.
Time to peak after single dose: Intravenous: 12 to 60 minutes; Intramuscular: 2-8 hours.
Volume of distribution: Neonates and young infants: 0.8-1.0 L/kg; Adults: 0.42-0.73 L/kg.
Main routes of elimination: 9-33% (average 23%) of the dose is excreted unchanged in urine. The remainder undergoes hepatic N-glucosidation and oxidation (CYP2C9 with a minor role of CYP2C19 and CYP2E1) followed by conjugation.
Elimination half-life (hours): Neonates: 43-217; Infants (1-12 months): 63.2+4.2; Children: 37-198; Adults: 75-126.
Plasma clearance (mL/h/kg): Neonates: 2.7-10.7; Children: 5.3-11.3; Adults: 2.1-4.9.
Protein binding: 45-60%.
Active metabolites: None.
Bioavailability: Intravenous: 100%; Intramuscular: 101 ± 11%.
Time to peak after single dose: Intravenous: 12 to 60 minutes; Intramuscular: 2-8 hours.
Volume of distribution: Neonates and young infants: 0.8-1.0 L/kg; Adults: 0.42-0.73 L/kg.
Main routes of elimination: 9-33% (average 23%) of the dose is excreted unchanged in urine. The remainder undergoes hepatic N-glucosidation and oxidation (CYP2C9 with a minor role of CYP2C19 and CYP2E1) followed by conjugation.
Elimination half-life (hours): Neonates: 43-217; Infants (1-12 months): 63.2+4.2; Children: 37-198; Adults: 75-126.
Plasma clearance (mL/h/kg): Neonates: 2.7-10.7; Children: 5.3-11.3; Adults: 2.1-4.9.
Protein binding: 45-60%.
Active metabolites: None.
A: Despite a decline in its popularity, at least in Europe and North America, phenobarbital should be considered a highly cost-effective treatment for early and established SE, not only in resource-limited settings. It also offers rapid and long-lasting action, a broad spectrum of efficacy (except for absence status), is easy to use, and is stable in solution.
A: Phenobarbital is considered an alternative to benzodiazepines for severe alcohol withdrawal due to its direct activation of the GABA receptor and its antiglutamate properties, which involve inhibiting glutamate response at NMDA receptors. This mechanism of action is advantageous because it is not affected by alterations to the GABA receptor that can result from chronic ethanol use and lead to benzodiazepine resistance. Furthermore, phenobarbital has a longer half-life (around 80 hours) compared to lorazepam (approximately 14 hours), which can lead to a self-tapering effect. Its less frequent administration may also reduce the risk of oversedation caused by dose stacking.
A: nappropriate use of Phenobarbital can lead to addiction and suicide attempts, which makes it a critical compound in forensic medicine.
A: The therapeutic concentration of Phenobarbital (PB) is typically maintained in the range of 15-40 µg/L to ensure its efficiency while preventing the risk of side effects.
A: Accurate monitoring of Phenobarbital (PB) is highly recommended to prevent side effects, considering its narrow therapeutical range.
A: Long-term utilization of Phenobarbital can lead to hyperactivity, sedation, behavioral problems, and dementia, depending on the dose.
A: Phenobarbital (PB) is known for its sedative and anticonvulsant characteristics, making it a critical agent for the management of epilepsy and seizure disorders. It is also a derivative of barbituric acid with hypnotic and sedative properties, recommended by the World Health Organization (WHO) as the first choice for treating epilepsy.
A: Phenobarbital (PB) is used in the treatment of neonatal jaundice because it can enhance the liver's drug metabolism, promote bilirubin metabolism, and ultimately reduce plasma bilirubin concentration, thereby achieving an anti-jaundice effect. It can also induce hepatic drug enzymes, which can promote the effects of other medications when used in combination.